At the heart of Internal Family Systems (IFS) therapy lies a deceptively simple yet radical idea: all parts are welcome.Even the ones that frustrate us. Even the ones we wish would just go away. Especially those.
When we begin inner work, it’s tempting to want to "fix" ourselves—to silence the anxious part, get rid of the angry one, or bury the wounded child. But IFS therapy invites us to take a different path: one of compassionate curiosity. One where healing doesn’t come from control, but from connection.
What Does Self-Compassion Look Like in IFS?
Self-compassion in IFS isn’t just about being nice to yourself. It’s about recognizing that every inner part—even the critical, chaotic, or exhausted ones—developed for a reason. They carry wisdom, history, and protective instincts.
When you lead with Self-compassion, you:
- Witness parts without judgment
- Invite them to share their fears and needs
- Offer calm, confident leadership without forcing change
This gentle leadership allows parts to unburden and transform naturally over time.
Why “Bad” Parts Aren’t Bad at All
Let’s take the inner critic. It may sound harsh. But when approached with curiosity, you might discover it formed to motivate you after a painful childhood failure. Or to prevent you from being embarrassed again.
The same goes for procrastination, anger, or emotional shutdown. These aren’t character flaws. They are coping mechanisms. By welcoming these parts instead of exiling them, you change your relationship to yourself. You foster trust.
From Fragmentation to Integration
Many people live with an inner landscape filled with conflict. One part says you’re too much. Another says you’re not enough. A third says you should just try harder.
Without Self-compassion, these voices become noise. But when you bring calm, curious presence to each one, you begin to hear what’s underneath:
- The pain of being judged.
- The fear of being abandoned.
- The longing to be accepted.
IFS therapy helps you connect these fragments and move toward internal integration. And integration isn’t perfection. It’s peace.
What Happens When All Parts Are Welcome
Something beautiful occurs when all parts feel heard:
- The inner critic softens into the protector.
- The exhausted child rests without guilt.
- The achiever learns to pause without fear.
The system becomes less chaotic, less reactive. More fluid. More trusting.
In time, your parts no longer battle for control. They learn to trust your Self to lead.
Daily Ways to Practice Self-Compassion
You don’t need to set aside hours for deep inner work. Self-compassion can start small:
- When you mess up, say: "A part of me is really disappointed. I wonder what it needs right now?"
- When you're anxious, ask: "What part is scared, and how can I support it?"
- When you're angry, whisper: "I see you. I know you’re trying to protect me. I’m here."
Final Thought: You Are the One You've Been Waiting For
IFS therapy is powerful not because it fixes you, but because it reconnects you with yourself. You become the one who can listen, love, and lead. You become the safe space you’ve always needed.
So let this be your mantra: All parts are welcome.
Yes, even the ones you’ve spent years trying to silence. Yes, especially those.
Because healing doesn’t begin with rejection. It begins with welcome.
And when you welcome all parts, you begin to come home to yourself.
One of the most valuable gifts of Internal Family Systems (IFS) therapy is its practicality. It doesn’t just explain your inner world; it gives you tools to heal it in real-time.
If you’ve ever felt stuck between two strong inner urges—like pushing through or giving up, staying silent or exploding, striving for perfection or collapsing into despair—then you know what inner polarization feels like.
IFS teaches us that when these parts speak up, we don’t need to silence them. We need to pause and listen.
The Inner Tug-of-War: An Everyday Experience
Here’s a familiar example:
- One part says: "Get up. Be productive. You'll feel better."
- Another says: "Lie down. You never get a break. You're exhausted."
Most people respond by aligning with one voice and suppressing the other. But what if you could talk to both?
A Real-Time IFS Check-In
This practice works especially well when you feel overwhelmed, stuck, or emotionally torn. All it takes is a few quiet moments, honesty, and curiosity.
Step 1: Pause and Breathe
Close your eyes. Take a few slow breaths. Let go of the need to fix or rush. Just be.
Step 2: Name the Voices
Identify the parts that are showing up. What are they saying? Give them names if it helps: "The Pusher," "The Protector," "The Tired One."
Step 3: Unblend from the Parts
You are not these parts. You are the Self—the compassionate witness who can listen without getting overwhelmed. Say to yourself: "I am the Self, and I welcome all parts."
Step 4: Start the Dialogue
Speak to each part in turn:
- "Thank you for trying to help me."
- "What are you worried might happen if I don’t listen to you?"
- "What do you really need from me right now?"
Let them answer in their own words. Don’t rush to judge or correct. Just listen.
Step 5: Validate and Lead
Let each part know it’s been heard. Then, as the Self, offer leadership:
- "I understand you're trying to protect me. I’m here to care for us now."
- "We don’t have to do it all or shut down completely. Let’s find a middle way."
What This Practice Does
This simple check-in defuses inner conflict without repression. It invites connection and clarity. It builds trust between your parts and your Self.
Over time, you may notice:
- Less internal tension
- More emotional resilience
- A deeper sense of self-trust
You begin to move through life not by force, but by inner collaboration.
A Journal Prompt to Deepen the Practice
Try journaling from the voice of each part. Let them take turns on the page. Don’t filter. Just let the voices speak. Then, respond from the Self.
You might be surprised at what surfaces—and what softens.
Final Thought: The Power of Presence
Real-time healing isn’t about fixing yourself. It’s about creating a space where all parts feel safe, seen, and supported.
When you pause and listen, you send a message to your inner system: I care. I’m here. I can handle this.
And in that space, healing begins.
People usually don’t connect problems with self-esteem and identity in adulthood to trauma on their own. They talk about indecision. Chronic self-doubt. Trouble asserting themselves. Feeling unsure of who they are, along with what they want. They tend to describe these issues as personal weaknesses - personality flaws, so to speak. In therapy, those explanations rarely hold up because it becomes obvious that trauma shapes self-esteem. Most of the time, these patterns have a history. They didn’t appear randomly in adulthood. They formed early and became defense mechanisms because they helped the person function in an environment that required constant adjustment. What looks like a self-esteem problem now often began as a way to keep relationships stable or avoid harm.
How trauma forms without a single event
Many adults dismiss trauma because they can’t point to anything dramatic happening to them. There was no accident. No abuse they recognize as abuse. No clear before-and-after moment. Childhood may even be described as “fine” or “normal.”
That doesn’t rule trauma out. Trauma doesn’t include extreme situations only. Rather, it’s defined by repeated exposure to situations where expressing yourself felt unsafe, unwelcome, or risky. That can include:
● emotional neglect
● chronic criticism
● inconsistent caregiving
● households where conflict either exploded or was never allowed
It can also include environments where a child had to take on adult responsibilities early or monitor other people’s moods closely.
When these conditions repeat, children adapt. They learn what keeps things calm. They learn what creates problems. And they learn when to speak and when to stay quiet.
These lessons aren’t learned consciously. They’re learned through repetition. Over time, they become automatic.
How early adaptation becomes a long-term pattern
The problem with early adaptations is that they don’t expire on their own. The nervous system doesn’t check whether circumstances have changed. It keeps responding based on what worked before. Later on in life, this may show up as emotional reactions that feel out of proportion or hard to control. Minor feedback can feel threatening. Conflict can trigger avoidance, compliance, or shutdown. Some people struggle to access their emotions at all.
Trauma doesn’t live as a clear memory you can think through and resolve. It shows up as patterns in how you regulate emotion, how you relate to others, and how you evaluate yourself, causing issues in how you think about yourself and others. In some cases, mental health issues can lead to destructive patterns like isolation, risky choices, substance misuse, or addiction. When experiences aren’t processed, unresolved trauma can cause overwhelming pain that stays mostly internal. That pain influences how you cope, how you manage emotions, and how you judge your own worth. Many people handle it indirectly, through overworking, self-criticism, control, numbing behaviors, or constant distraction. These strategies help in the short term, but they also reinforce the underlying patterns.

The impact of trauma on self-esteem and identity in adulthood
Self-esteem develops through experience, not reassurance. It grows when a person is treated as someone whose needs matter, when mistakes don’t threaten the connection, and when approval isn’t conditional.
Trauma interferes with those experiences. If safety or acceptance depended on being useful, agreeable, competent, or emotionally contained, self-worth becomes conditional. The person learns that value has to be maintained.
This often shows up in adulthood as constant self-monitoring. There’s a sense of being evaluated even when no one is paying attention. Praise doesn’t settle. Rest feels uncomfortable. Mistakes feel costly. This isn’t simply low confidence. It’s unstable self-esteem that depends on external conditions.
How trauma affects identity development
Identity develops through exploration. Trying things. Being wrong. Changing your mind. Being seen without consequences. Now, when survival matters more than self-expression, identity takes a back seat. The person becomes what the environment requires. Responsible. Adaptable. Low-maintenance. Useful.
Those roles often continue into adulthood because they still work. They reduce conflict. They keep relationships intact.
But they don’t answer basic questions. What you want. What you value. And what feels meaningful.
Work on early trauma and attachment points to a similar pattern: ongoing stress in childhood can interfere with how people learn to read situations, manage emotional reactions, and feel secure with others. When those skills don’t have a chance to develop consistently, the sense of self that forms later is often shaky. Childhood trauma is also linked to more anxious or avoidant relationship patterns, lower self-regard, and difficulty forming a clear picture of who you are that can carry into adolescence and adulthood.
How relationships reinforce trauma-based identity
Trauma-related patterns show up most clearly in relationships. If your sense of self developed around monitoring others, relationships become the primary source of stability. Approval feels grounding. Distance or conflict feels destabilizing.
Some people cope by accommodating excessively. Others cope by avoiding closeness altogether. Both are attempts to manage uncertainty.
In either case, identity remains reactive. It changes based on context rather than internal continuity. That
instability feeds back into self-esteem and reinforces reliance on external feedback.
How trauma-informed work supports repair
Repair comes from building tolerance for internal experience - learning to notice reactions without immediately acting on them, and allowing needs and preferences to exist without justification.
In therapy, this often involves paying attention to moments where old patterns activate. Noticing the urge to explain, minimize, or self-correct. Staying with the discomfort long enough for something new to happen.
Over time, consistent experiences of being taken seriously and having boundaries respected create internal stability. Self-worth becomes less conditional. Identity becomes less role-based.
Not perfect. Just more stable.
Final thoughts
Trauma shapes self-esteem and identity in adulthood because adaptation was necessary early on. Those adaptations worked. That’s why they lasted. Understanding this doesn’t erase the impact. It changes how the patterns are interpreted. Instead of evidence of something wrong, they can be understood as responses to conditions that no longer exist. Many people find that shift is the first step toward meaningful change.
In IFS therapy, not all parts speak with the same volume. Some whisper, some analyze, some push us into overdrive. But there is one voice that often shouts with urgency, fatigue, or frustration—a voice many of us learned to ignore: the inner child.
This part isn't metaphorical. It's real. The inner child is a part of you frozen in time, holding onto pain, unmet needs, or emotional truths from your early years. It's often one of the loudest parts in your system because it carries the rawness of wounds that were never healed.
Childhood Wounds and the Rise of Protector Parts
When we experience pain, neglect, or emotional overwhelm in childhood, our system adapts. We create protector parts to help us survive. These may include:
- The Perfectionist, who learned that mistakes led to punishment.
- The People-Pleaser, who kept peace to avoid conflict.
- The Achiever, who tied their worth to accomplishments.
These parts formed not to hurt us, but to protect the wounded child within—the one who felt unsafe, unseen, or unloved. In IFS therapy, these are called manager parts because they manage our lives to prevent the inner child from being triggered.
Then there are the firefighters, the parts that spring into action when the inner child is activated. They might distract you with binge-watching, overeating, or numbing out. Again, their motive is protection.
But beneath both managers and firefighters lies the exiled part — the Wounded Inner Child.
Who Is the Wounded Child?
The Wounded Child part carries:
- Grief from not being comforted when they were scared
- Anger from being ignored or misunderstood
- Shame from being criticized or rejected
This part often emerges during emotional flashbacks, moments when our reaction seems far bigger than the situation. That's the child inside, finally having space to speak.
You may hear this part say things like:
- "This isn’t fair!"
- "Why doesn’t anyone care about me?"
- "I just want someone to help."
It might manifest through tears, tantrums, or deep exhaustion. And for many, the instinct is to silence it—to "get it together" or "move on."
But in IFS, we do something radical instead: we listen.
Creating Space for the Inner Child’s Voice
Healing begins when we stop suppressing and start witnessing. When we turn toward the loud, hurting part and say, "I'm here now. Tell me everything."
Here’s how to begin:
- Notice Emotional Intensity: When your reaction feels out of proportion, pause. Could this be a younger part surfacing?
- Get Curious: Ask, "How old does this part feel? What is it trying to say?"
- Unblend: Remind yourself: "I am not this overwhelmed part. I am the Self who can listen with love."
- Offer Compassion: Speak to the inner child as you would to a real child. Use gentle words. Offer comfort.
- Make Time: Journal, draw, or talk aloud to let the child express. They may need more than one invitation to feel safe enough to share.
The Power of Being Heard
The inner child doesn't need you to fix the past. They need to feel seen in the present.
By creating space for their voice, you begin to release the burden they've been carrying. You help your protector parts realize they no longer have to shield you so rigidly. And you deepen your trust in your own capacity to lead from Self.
Final Thought: All Voices Matter
IFS therapy teaches that healing happens not through silencing parts but through integration. Every part—even the angry child, the scared one, the one who wants to shut it all down—deserves a voice at the table.
You don’t have to fear the loud parts. They’re just trying to be heard. And when you listen with love, they begin to heal.
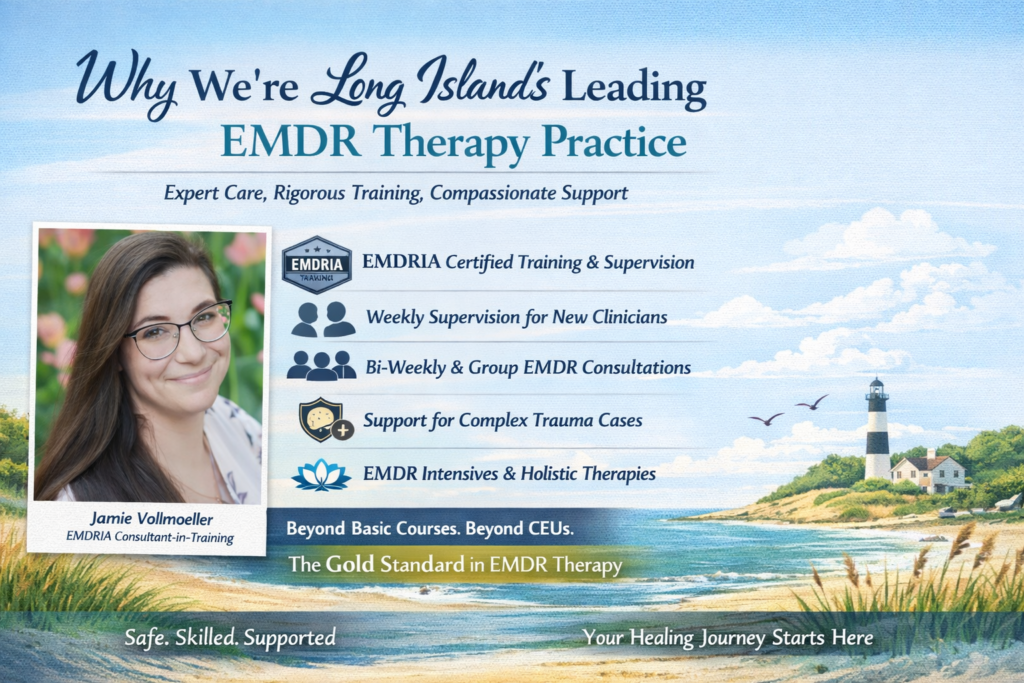
When you're ready to begin trauma healing, the thought of working with a clinician newer to EMDR can raise valid questions: Will they understand my experience? Will EMDR be safe for me? What if my trauma is too complex?
At our Long Island-based EMDR therapy practice, we've built a system that not only acknowledges these concerns—but resolves them with care, structure, and deep clinical oversight.
Here’s how we do things differently:
✅ Clinicians Trained Through EMDRIA—the Gold Standard
All our therapists receive EMDR training through EMDRIA, the official credentialing body for EMDR therapy. EMDRIA’s standards are internationally recognized and require intensive coursework plus ongoing consultation with an EMDR-certified supervisor. This stands in stark contrast to other options like PESI or brief certification courses, which may offer quick CEU credits but lack supervision, case review, and skill development support.
At our practice, EMDR isn’t a checkbox—it’s a deeply supported, continually monitored modality.
✅ Clinical Safety Comes First
Every clinician learning EMDR works under the close guidance of our founder, Jamie Vollmoeller, an EMDRIA Consultant-in-Training. Newer clinicians meet weekly for supervision and do not begin EMDR trauma processing until Jamie has reviewed the case and confirmed client readiness.
✅ Complex Trauma? You’re Never Alone
For clients with layered or complex trauma histories, therapists have real-time access to expert consultation and are trained in additional nervous system regulation techniques like Polyvagal Theory and Internal Family Systems (IFS) to ensure safety and effectiveness.
✅ You’re Not a Training Case
Our clinicians are not interns. They are licensed or provisionally licensed professionals committed to excellence. Supervision enhances their clinical depth—it doesn’t substitute for it. Your healing journey is treated with the highest level of professionalism and care.
✅ Seamless Continuity of Care
You’ll work with your clinician throughout your journey. Supervision means your therapist has a team behind them—not that you'll be passed from one provider to another.
✅ Growth Backed by Community
Once past the initial 6-month EMDR onboarding, clinicians continue to receive bi-weekly supervision and monthly EMDR group consultation. That means every EMDR therapist here is continually refining their skill—and your care benefits from that evolution.
✅ EMDR Intensives Available
For those seeking deeper healing, we also offer EMDR intensive sessions—with the same trauma-informed, regulated, and supervised support.
If you're looking for safe, expertly guided EMDR therapy in Long Island, our team is ready to walk with you—no matter where you are in your healing.
In the world of IFS therapy (Internal Family Systems), one of the most relatable and revealing dynamics is the experience of polarized parts. Have you ever felt two voices inside you pulling in opposite directions? One pushes you to stay busy and productive, while another pleads for rest and silence? That inner tension isn't unusual—it's actually a core concept in IFS therapy.
What Are Polarized Parts in IFS Therapy?
In IFS therapy, polarized parts are internal subpersonalities that oppose each other, often battling for control in your emotional system. These parts form over time, usually as responses to past wounds or learned survival strategies. While their methods may seem contradictory, their intentions are often protective.
For example, the part that insists you "get up and go" may be trying to preserve your sense of worth, while the part that says "lie down and rest" is seeking to protect you from burnout or emotional pain. The conflict isn’t sabotage—it’s self-protection in action.
Why Do Polarizations Happen?
Polarization happens when two or more parts get locked into opposing strategies for protecting the system. This often develops from unresolved pain or trauma. Without access to Self-leadership, these parts are left to fend for themselves, trying to take over based on old scripts:
- The Achiever says, "You’re only safe if you succeed. Keep going."
- The Exhausted Inner Child says, "I can’t do this anymore. I just want someone to care."
Over time, this back-and-forth becomes exhausting and confusing, leading people to feel overwhelmed or broken. But IFS therapy reframes this: you're not broken—you're internally divided, and all parts are trying to help in their own way.
Common Polarized Parts You Might Recognize
Here are some everyday examples of polarization:
- Push Through vs. Shut Down: One part demands productivity, the other resists with fatigue or numbing behaviors.
- Speak Up vs. Stay Silent: A part wants to assert boundaries, while another fears rejection or punishment.
- Please Others vs. Prioritize Self: One part wants connection, the other wants independence.
Healing Polarized Parts with IFS Therapy
The beauty of IFS therapy is that it doesn’t ask you to choose a side. Instead, it teaches you to listen to both voices from a place of Self-energy — the calm, compassionate presence within you that isn’t fused with any one part.
When you access the Self, you become a mediator. You let each part share its story, its fears, and its hopes. And in that space of witnessing, something powerful happens: the tension begins to dissolve. The parts soften, realizing they no longer have to fight for dominance. They can trust the Self to lead.
A Real-Life Check-In: Self-Led Dialogue with Polarized Parts
Try this when you feel torn:
- Pause and Identify the two voices. E.g., "Get up and hustle" vs. "Please stop and rest."
- Unblend from both. Remind yourself: "I am not these voices. I am the Self who is listening."
- Speak to Each Part:
- "Thank you for trying to protect me."
- "What are you afraid would happen if I didn’t listen to you?"
- "What do you need right now?"
- Listen. Let them answer in their own tone and words. No need to fix, just hear them out.
- Lead with Self. Reassure both that their concerns are valid, and you will care for the system as a whole.
You Don’t Have to Be at War Inside
Polarized parts are not flaws to fix. They're signals to understand. Through IFS therapy, we learn to navigate inner conflict not by suppressing it, but by honoring it.
The goal isn't to pick winners. It's to create internal harmony.
And when that happens, even the loudest voices begin to trust. Even the most exhausted parts begin to rest. And you begin to lead your life from a place of peace.
Some days, it feels like we’re made of many voices, each pulling us in different directions. We try to stay productive, but fatigue weighs us down. We yearn to rest, but guilt holds us hostage. One part of us whispers encouragement, while another screams for relief. It’s a common, deeply human experience—and one that Internal Family Systems (IFS) can help us understand and heal.
IFS, developed by Dr. Richard Schwartz, introduces a powerful idea: you are not a single, monolithic identity. Instead, you are a complex system made up of different "parts" that carry their own thoughts, feelings, and intentions. At the core of this system is the Self—a calm, compassionate, curious center that has the innate ability to lead with clarity and care.
We Are Multidimensional, Not Broken
The first and perhaps most radical teaching of IFS is that you are not broken. All those conflicting thoughts, all those emotional ups and downs, are not signs of dysfunction. They are signs of multiplicity. We contain multitudes.
Think of your inner world like a family. There are parts that are strong-willed and always pushing you to achieve. There are parts that want to protect you from rejection or shame. There are parts that carry old wounds—the child within who never felt safe, who never got to speak. And there is also a Self: the wise, grounded presence within you capable of holding space for them all.
When we feel inner conflict, it's often because different parts are trying to protect us in their own way. For example:
- The Achiever may push you to work harder out of fear of failure or being seen as not enough.
- The Comfort Seeker may urge you to rest or numb out with food, social media, or sleep to avoid pain.
- The Inner Critic may bombard you with harsh words, not because it hates you, but because it fears you'll be hurt if you let your guard down.
- The Wounded Child might throw tantrums or withdraw when it feels unseen or overwhelmed.
None of these parts are bad. They each developed for a reason, often in response to past experiences where we needed to adapt or survive. IFS invites us to meet them with curiosity rather than criticism.
The Calm Self at the Center
At the heart of the IFS model is the belief that we all have a Self—a steady, loving inner leader. The Self is not a part, but the one who can relate to all parts with compassion and clarity. When the Self is leading, we feel the 8 Cs: calm, clarity, curiosity, compassion, confidence, courage, creativity, and connectedness.
You may have glimpsed your Self when you felt at peace despite chaos, when you responded to your own pain with kindness instead of judgment, or when you were able to witness a difficult emotion without being overwhelmed by it.
The goal of IFS work isn’t to eliminate or fix your parts. It’s to help them trust the Self to lead. When parts feel heard and respected, they often soften. Their roles can shift from protection to support.
Meeting Your Inner Team
Start by simply noticing your parts. When you’re triggered, anxious, or exhausted, ask yourself:
- What part of me is speaking right now?
- What does this part want for me?
- What is it afraid might happen?
You may be surprised by the wisdom that emerges. Journaling or speaking out loud can help externalize the internal dialogue. For example:
- "I hear the part of me that wants to keep pushing. It believes I need to stay productive to be valued."
- "I see the part that just wants to curl up and rest. It's tired from carrying the load for so long."
These voices don’t need to be silenced. They need to be witnessed.
Healing Begins With Curiosity, Not Control
So often, we try to manage ourselves through force. We criticize the lazy part, ignore the anxious part, or suppress the angry part. But IFS offers a gentler way. It says: what if these parts are not enemies, but messengers?
What if every reaction, no matter how confusing or frustrating, is an attempt to help you—even if it's a misguided one?
When we turn toward our parts with compassion, we stop the inner war. We begin to understand how our internal system came to be, and how we can gently shift it toward harmony.
You Are Not Alone Inside
This shift in perspective—from seeing ourselves as broken to seeing ourselves as beautifully complex—is profoundly healing. It allows us to hold space for our contradictions. To offer grace to the parts that are scared. To lead our inner system from the Self.
In IFS, healing is not about erasing the past. It’s about understanding how it shaped our parts and allowing them to release burdens they were never meant to carry.
You are not broken. You are a system of protectors, survivors, and a Self that can lead them home.
Grief changes everything. It slows the body, bends the mind, turns days into long corridors with no exit signs. People will reach for comfort in different ways. But – not every option brings substantial, healthy relief. Some might turn to food, some to silence, some to substances that cloud the pain rather than easing it. The process of preventing substance reliance in mourning means finding safer anchors while still allowing sorrow to move through your body and mind. The absence of one person shouldn’t result in the absence of ourselves.
Subtle Warnings
Grief often starts with numbness, and then the numbness demands filling. A glass of wine quickly becomes two. Sleep comes through medication, not real rest. These changes are initial indicators of substance use. They may seem minor at first, but in reality, they are early signs of substance use that families tend to overlook. That’s because relying on substances in grief is sometimes considered normal. What began as coping might harden into reliance. The trick is to notice patterns before they cement.
Warnings are usually hiding in plain sight. Prescriptions that run out weeks early. Excuses that sound thinner with each retelling. A loved one insists they’re doing fine, though their skin dulls and their energy fades. Watch out for these markers of a deeper struggle.

Friends as a Safety Net
Some losses create silence inside the house. Friends can fill that silence with stories that will keep the memory alive. Leaning into trusted connections stops grief from looping inward. A shared walk, a call at midnight, even watching a bad TV movie together can put together a fragile mind. Friends carry us into the present when the past feels heavier than the body’s able to hold.
\Friends see what we can’t and can provide a different perspective and social support. They can notice the drop in appetite, the missed appointments, and the increasing distance from hobbies you used to enjoy. They remind us that life still asks for our participation.
There’s no perfection in friendship during grief. Some friends might say clumsy things. Others will offer silence that feels more like absence. Still, it’s the attempt that matters. Even a flawed presence can ground someone who feels unmoored.
Guidance Beyond Familiar Faces
There are days when friends don’t know what to say, or when their comfort feels thin. Professionals – therapists, counsellors, support groups for people in mourning – stand ready. They hold space for questions that might frighten or concern family members. Their guidance is there to shape grief into something less wild, less consuming.
Professional guidance offers much-needed structure to days spent in mourning. Therapy sessions create steady appointments that counter the drift of grief. Support groups or grief and loss counselling will replace isolation with shared recognition, reminding mourners they’re not alone or unique in their pain. Clinical care adds practical strategies – breathing exercises, journaling prompts, cognitive reframing –
that turn abstract emotions into manageable pieces.
The Unfiltered Voice
Emotions we leave to silence tend to ferment. Speaking them aloud – shame, anger, sadness – releases pressure before it’s turned into collapse. Some find it easier to write letters they’ll never send, or to scream in the car on the drive home. Others will talk through tears with someone who listens without judgment. Grief demands air. Holding it back stiffens the body and sharpens the pain. Expressing it keeps the system from shutting down.
Words act as safety valves. Journals capture thoughts too jagged for conversation. Recordings on a phone preserve confessions meant for no one’s ears but our own. A painting, a song, or even an angry rant in the shower becomes testimony to what the body refuses to carry alone.
Families can sometimes resist this openness. They might urge mourners to be strong. Yet strength is a myth if defined by silence. Releasing emotion, in raw form, reclaims power. It ensures grief doesn’t calcify inside the chest.

The Shape of Rituals
People have always used rituals to survive loss. Lighting a candle every morning, cooking the favorite meal of the one gone, or setting aside a song for Sunday afternoons – each action anchors memory in a repeatable form. Rituals are a fundamental part of the human experience; among other things, they structure grief. With structure, sorrow feels less formless, less endless.
Rituals also carry culture. They connect us to generations that came before, reminding us that mourning is shared across time; nothing new under the sun. That connection provides reassurance that grief is survivable because others have already walked the path. Rituals are reliable ways of preventing substance reliance in mourning.
The Body Remembers Too
The mind spirals in mourning, but the body needs equal attention. Eating food that sustains energy, sleeping enough hours, and moving in simple routines prevent the body from collapsing under the weight of loss. A healthy body can also steady the grieving mind. Without it, sadness deepens into illness.
A mourner who skips meals loses the energy they need to handle emotional storms. Sleep deprivation will only magnify sadness and might lead to despair. Ignoring physical needs reduces resilience. This kind of personal neglect will leave the person more vulnerable to unhealthy coping.
In grief, acts of self-care may feel a little trivial. However, drinking water, stepping into a shower, brushing teeth – these signal continuity of life. They serve as reminders that the body still belongs to us, even when the heart feels broken.
Air and Motion
Stepping outside resets perspective. Fresh air clears thoughts, and exercise releases tension. Walking a park path, stretching in the yard, or biking through quiet streets turns grief into motion instead of stasis. The body in motion keeps the mind from becoming locked in a single story of loss. And somewhere on the path, breath somehow feels easier again.
Exercise need not be intense. A slow walk around the block might be enough. Gardening places hands in soil, reminding us of cycles larger than our individual lives. Even standing under the clear open sky, breathing deeply for minutes at a time, will restore balance.
The outdoors also reconnects us with community, one of the oldest defense mechanisms out there. Neighbors wave. Children laugh in playgrounds. Strangers walk dogs past us. These fragments of normal life weave back into our perception. They’re showing us that continuity exists beyond grief.
Holding Steady
Grief is heavy, but it doesn’t necessarily have to drag someone into dependency. The real work lies in weaving support, ritual, and movement into daily life. It lies in staying alert to signals that something else, something unhealthy, is taking over. Preventing substance reliance in mourning is also giving grief its time without letting it consume every part of existence. In that balance, memory remains intact, and life,
though altered, continues forward, as it should.

Bringing a new life into this world is an awe-inspiring moment that's often clouded by the unanticipated emotional turmoil of postpartum depression (PPD). If you find yourself feeling unusually despondent, anxious, or overwhelmed after giving birth, it's crucial to recognize that you're not alone in this struggle. Understanding the fine line between normal hormonal changes and symptoms of PPD is the first step toward healing. This guide is designed to walk you through the maze of emotions and help you find your footing again.
Understanding the Normal Hormonal Roller Coaster
The days and weeks following childbirth are a tumultuous time for a new mother's body, largely due to the dramatic hormonal shifts that occur. After delivery, estrogen and progesterone levels, which were significantly elevated during pregnancy, rapidly decline to their pre-pregnancy states. This swift change can significantly impact a mother's emotional and mental state, contributing to mood swings, feelings of sadness, and irritability. These symptoms, often referred to as the "baby blues," are a common experience for many new mothers as their bodies attempt to recalibrate. While unsettling, these feelings are typically short-lived, usually resolving within the first two weeks postpartum. It's crucial for mothers to recognize these hormonal fluctuations as a normal part of the postpartum period, understanding that these emotional responses are a direct result of their body's natural adjustment process.
Identifying the Signs of Postpartum Depression

Identifying the signs of postpartum depression requires a discerning eye, as its manifestations can be far more severe and persistent than those of the typical post-birth hormonal adjustments. Symptoms that might indicate the onset of PPD include a pervasive sense of despair, intense anxiety, or a profound detachment from your newborn, which might feel like an insurmountable gap. You may find yourself struggling with an overwhelming sense of inadequacy as a mother or harbor intrusive thoughts of harm towards yourself or your baby.
Unlike the transient nature of the "baby blues," these feelings linger well beyond the initial two weeks following childbirth. Recognizing these symptoms as potential indicators of PPD is a crucial step in advocating for your mental health. It’s imperative to understand that such experiences, while deeply distressing, are not reflections of your capability or love as a mother but signals that you may need support and treatment to navigate this challenging period.
When and How to Seek Help
If feelings of despair, intense anxiety, or detachment persist beyond the initial weeks following childbirth, it's imperative to initiate a conversation with a healthcare professional. This crucial step can pave the way to receiving the comprehensive care necessary for recovery. A doctor or mental health specialist can offer a tailored approach to treatment. This may encompass therapy sessions, medication, or a blend of both, depending on the individual's specific needs. Additionally, it's beneficial to openly discuss your experiences with close ones. Sharing your struggles not only fosters a supportive environment but also demystifies the challenges of PPD. It will encourage a collective effort in your recovery process. Engaging in dialogue about your feelings is not an admission of failure. It's a proactive measure towards reclaiming your well-being. Remember, seeking assistance is a proactive gesture of self-care and an important milestone on the path to healing.
Building Your Support System

Creating a strong network of support is crucial for mothers facing the challenges of postpartum depression. Identifying those in your life who can offer practical and emotional assistance is vital. Family members, friends, and even neighbors who understand what you're going through can be invaluable resources. They can provide a listening ear, share experiences, or help with daily tasks. This will make it easier for you to focus on recovery.
Consider joining a support group for new moms, where you can connect with others who are navigating similar experiences. These groups offer a safe space to express feelings and share coping strategies. Additionally, leveraging online communities can also provide support and information at any time of the day. It can make it easier to find encouragement even during late-night feedings. Embrace the help offered by those around you; it's a sign of strength to accept support when you need it the most.
Exploring EMDR Therapy
EMDR (Eye Movement Desensitization and Reprocessing) therapy has been gaining traction as a notable option for managing symptoms of postpartum depression, especially for individuals who have experienced traumatic events. This form of psychotherapy utilizes bilateral stimulation, such as guided eye movements, to help patients process and integrate distressing memories and traumas that may be contributing to their current emotional state.
For mothers grappling with PPD, EMDR offers a pathway to address underlying traumas that might be exacerbating their symptoms. This will facilitate a deeper healing process. It's essential to consult with a mental health professional skilled in EMDR to assess its suitability for your specific situation. This therapy is not a one-size-fits-all solution. For many, it provides a valuable tool in the recovery toolkit. This can offer a ray of hope for those feeling ensnared by the grip of postpartum depression. Engaging in EMDR could be a pivotal step toward emotional resilience and a more positive postpartum experience.
Self-Care Strategies for Managing Symptoms

Incorporating self-care into your routine is pivotal when navigating the complexities of postpartum depression. Focusing on nutrition by choosing balanced, nourishing meals can significantly impact your overall mood and energy. Engaging in physical activity can uplift your spirits and improve mental clarity. Even if it's a short walk around the neighborhood! Prioritize sleep whenever possible; although challenging with a newborn, seizing moments for rest can be rejuvenating. Carve out time for activities that replenish your soul, whether it's reading, soaking in a warm bath, or practicing mindfulness.
Even brief moments of self-indulgence can foster a sense of normalcy and personal well-being. Embrace these practices not as luxuries, but as essential components of your recovery journey. Acknowledge that caring for yourself empowers you to care for your baby with renewed strength and positivity.
Navigating Relationships and Setting Boundaries
In the throes of postpartum depression, the dynamics of your relationships may shift, underscoring the importance of clear communication and the establishment of boundaries. It's essential to express your needs and limits to those closest to you during this sensitive period. Asserting what you're comfortable with, be it declining social visits when you're not feeling up to it or requesting specific types of help, is crucial for your emotional health. Encourage an open dialogue with your partner, emphasizing the need for mutual understanding and support. Remember, setting boundaries isn't about pushing others away. It is about safeguarding your well-being and creating a nurturing environment for both you and your baby. Recognize that it's healthy and necessary to ask for space or assistance, and those who genuinely support you will honor these requests without judgment.
The Power of Trust and Letting Go

Navigating the tumultuous waters of postpartum depression often requires a deep dive into self-trust and the acceptance of help from others. It's a journey that illuminates the importance of acknowledging our human limitations and the strength found in vulnerability. Embracing the fact that perfection is an unattainable standard. This can free you from the self-imposed pressure that compounds the stress of new motherhood.
Trusting in your inherent capabilities as a mother and allowing yourself the grace to make mistakes can significantly lighten the emotional load of PPD.
Additionally, relinquishing some control and entrusting others with tasks, even those involving your baby, can foster a healthier, more balanced environment for everyone involved. This act of letting go not only helps in redistributing the weight of responsibilities but also in strengthening the bonds of trust with those around you. The journey through PPD is one of gradual healing, learning, and growing stronger in the realization that it's perfectly okay to not have all the answers, and that reaching out and opening up is a sign of resilience, not weakness.

The journey of balancing pregnancy, work, and motherhood is akin to performing a high-wire act without a safety net. The stakes are high, and the fear of falling can be overwhelming. In this complex juggling act, pregnancy introduces a new level of challenge. This can stir up a mix of emotions and significantly amplifying anxiety. However, amidst the chaos, there's a path to harmony and well-being. Let's explore how to navigate this multifaceted journey with grace and strength.
Navigating the Emotional Rollercoaster of Pregnancy and Work

Embarking on the journey of pregnancy while managing a full-time career and existing family duties can often feel like navigating an emotional tempest. This period is marked by a complex blend of exhilarating highs and daunting lows. The anticipation of a new family member brings joy, yet the balancing act of work and personal responsibilities heightens anxiety.
To sail through these tumultuous waters, it’s essential to cultivate a mindset of flexibility and kindness towards oneself. Understand that it’s natural for energy levels and capabilities to fluctuate during pregnancy. Accepting this fact can lead to a more compassionate approach to self-expectations and workload management.
Embracing open communication with your employer about your needs and potential adjustments in your work environment or schedule is crucial. Likewise, building a support network that includes colleagues aware of your situation can provide a safety net for days when the balance feels particularly precarious. It’s about finding and implementing strategies that cater to your changing needs. It is also about ensuring that your health and the well-being of your unborn child are prioritized. By acknowledging the unique challenges of this journey and actively seeking solutions, you pave the way for a smoother transition through each trimester, fostering resilience against the backdrop of professional and personal demands.
The Unseen Battle: Anxiety, Depression, and Motherhood

The interplay between motherhood, pregnancy, and work often serves as a fertile ground for the development of anxiety and depression. The relentless pursuit of perfection in every aspect of life can spiral into a cycle of self-doubt, persistent overwhelm. This can lead to an eventual sense of burnout. It's imperative to recognize these emotions as a normal response to an exceptionally demanding set of circumstances. Early recognition of anxiety and depression symptoms is critical, allowing for timely intervention and support.
This phase can particularly intensify the challenge of managing everyday stressors, leading to an increased risk of experiencing feelings of not being good enough and a fear of losing control over one’s life. The pressure to maintain an unwavering façade of strength and composure only adds to the emotional load, making it harder to reach out for help. However, acknowledging these vulnerabilities can be transformative, setting the stage for a journey towards healing and equilibrium.
It's important to understand that these feelings do not define one's capabilities as a mother or a professional. They are, instead, indicators of the need for a more supportive environment and possibly professional help. Recognizing the signs and seeking assistance is a sign of strength, paving the way for recovery and a more balanced approach to the dual demands of work and family life.
Seeking Support: You Don't Have to Do It Alone

In the dynamic and often demanding journey of managing pregnancy, work, and motherhood, the strength found in community and support cannot be overstated. Acknowledging the need for help and actively seeking it is a testament to one's wisdom and resilience, not a mark of inadequacy. It’s crucial to lean into the networks available to you, whether they consist of family, friends, or professional resources. Opening up to a partner about the pressures you’re facing can create a shared understanding and collaborative solutions. Engaging with friends who uplift and encourage you can provide emotional respite and practical assistance. Furthermore, professional support groups or counseling services offer structured guidance and understanding from those well-versed in these challenges.
Embracing assistance allows for a redistribution of the load, making the path forward less daunting. It is through this sharing of burdens that a more balanced and sustainable approach to navigating this period becomes possible. By welcoming support, you not only fortify your own wellbeing but also model for your children the value of community and vulnerability. This journey, while uniquely yours, need not be a solitary one. The act of reaching out for help can illuminate the way, revealing a landscape of resources and allies ready to walk alongside you.
Setting Boundaries: The Art of Saying No

Mastering the art of setting boundaries is an invaluable skill in the labyrinth of pregnancy, work, and motherhood. It’s an act of self-preservation, a declaration that your well-being and that of your family take precedence. The essence of setting boundaries lies in discerning what truly merits your energy and attention. It is acknowledging that not all demands are equally deserving and that some may, in fact, detract from your ability to maintain balance and harmony in your life.
Embracing the power to say no is not about closing doors but about opening up space for what truly enriches you and your family. It’s an exercise in prioritizing, making conscious choices about where your time and energy are best invested. This may mean declining additional projects at work that conflict with your health or family time or opting out of social engagements that leave you more drained than fulfilled.
Learning to navigate these choices without guilt is critical. Society often glorifies busyness, equating it with importance or success. However, true strength lies in recognizing when less is more. By setting boundaries, you safeguard your mental and emotional well-being, ensuring that you remain resilient and energized. It is through these deliberate choices that you carve out a path that respects your needs and nurtures your family’s well-being.
EMDR Therapy: A Ray of Hope for Anxiety and Depression
EMDR Therapy, standing for Eye Movement Desensitization and Reprocessing, emerges as a promising solution for those grappling with the shadows of anxiety and depression amidst the whirlwind of pregnancy, work, and parenting responsibilities. This therapy operates on the principle of facilitating the brain's innate healing processes, particularly focusing on how traumatic memories and emotional distress are processed. Through guided eye movements and a structured approach, EMDR aids individuals in revisiting emotional disturbances in a safe and controlled environment.
What sets EMDR apart is its ability to delve into the root causes of emotional turmoil without the need for detailed discussion of the distressing events, making it a less verbally intensive yet profoundly impactful therapy. This aspect is especially beneficial for those who may find traditional talk therapies daunting or re-traumatizing. By reprocessing these memories and reducing their psychological impact, EMDR therapy fosters a significant decrease in the symptoms of anxiety and depression, paving the way for a clearer path to emotional well-being.
Incorporating EMDR therapy into a holistic approach to mental health can assist in unlocking a more balanced state of mind. It stands as a testament to the power of innovative psychological treatments in overcoming the complexities of emotional distress, offering a ray of hope to those navigating the intricacies of motherhood, pregnancy, and professional life.
Incorporating Self-Care into Your Daily Routine

In the whirlwind of balancing pregnancy, work, and family responsibilities, dedicating time to self-care becomes both a strategic move and a profound act of kindness to oneself. It's about identifying and integrating practices that replenish your energy and bring you joy, grounding you amidst the chaos. Consider simple pleasures and activities that resonate with your soul, whether it's indulging in a favorite book, enjoying a peaceful walk in nature, or savoring moments of solitude.
Mindfulness practices, such as meditation or deep-breathing exercises, can also be powerful tools in managing stress and enhancing your emotional well-being.
Physical activity, tailored to your body’s changing needs during pregnancy, can significantly contribute to your overall health and mood. It's not about rigorous exercise routines but finding joy in movement, be it through prenatal yoga, swimming, or gentle stretching. Moreover, ensuring adequate rest is paramount. Pregnancy and early motherhood can be physically demanding, making quality sleep and relaxation crucial for your body’s recovery and well-being.
By weaving self-care into the fabric of your daily life, you create a sustainable foundation that supports not only your health but also enables you to nurture your family with renewed energy and patience. This commitment to self-care is a reflection of your strength, allowing you to embrace each day with resilience and grace.
Trusting in Your Strength and Abilities
Amid the flurry of managing pregnancy, career demands, and nurturing a family, it's crucial to anchor yourself in the belief of your own strength and capabilities. This chapter of your life, teeming with its own set of hurdles and highlights, demands a deep-seated trust in your resilience and ingenuity. Embracing this period means understanding that you possess an innate power to overcome obstacles and forge a path that aligns with your values and aspirations.
It's essential to remind yourself that while the journey is challenging, it also highlights your incredible capacity to adapt and thrive. Each day presents an opportunity to learn, grow, and extend grace to yourself, recognizing that perfection is not the goal—progress and well-being are. Celebrate the small victories, for they are testament to your perseverance and dedication.
By cultivating a mindset that appreciates your efforts and acknowledges your achievements, you create an inner dialogue that supports and uplifts you. Let this trust in your abilities be the compass that guides you through moments of doubt or uncertainty. Remember, the journey of balancing pregnancy, work, and motherhood is not just about surviving but thriving, powered by an unwavering belief in your own strength and potential.